TalkingDrugs reached out to the winner of the SHI New Writer’s prize to speak a bit more about their research. This is a summary of the article published in the Sociology of Health & Illness: Drug fatalities and treatment fatalism: Complicating the ageing cohort theory. It was also discussed by the Society for the Study of Addiction here.
Opioid-related deaths in the UK have been increasing for nearly a decade. Older heroin consumers are particularly at risk, with the highest rates of deaths among people aged 40–49 and the steepest rises in the over-fifty age bracket. As such, a popular theory for the UK’s increase in opioid-related deaths (and by extension, drug-related deaths, more generally), made by the UK government, and propelled in the media, is that there is an ageing cohort of heroin users with age-related health complications predisposing them to an overdose. However, in this Wellcome Trust-funded study, I speak to those older heroin users deemed to be most at risk and get a very different story. Rather than positioning their age as a risk factor, participants cite many reasons why they feel their age is actually protecting them. This leads me to ask: If this risk of overdose and premature death is not perceived to be coming from a natural process of ageing and age-related health complications, where might it be coming from? With this, participants point us towards a treatment system that is failing to meet their needs.
Before I go into this argument further, let me just say something about this ageing cohort theory. This is the idea that we are experiencing higher rates of drug-related deaths because there is an ageing cohort of people who use heroin. For example, in Public Health England’s (2016) report, following their national enquiry into these steep rises in deaths, they note many factors, with “the principle one being an ageing cohort of 1980s and 1990s heroin users who are experiencing cumulative physical and mental health conditions that make them more susceptible to overdose” (2016: 14). Although rooted in these kinds of governmental reports, the theory has proved particularly popular in the local and global media, who have dubbed this cohort the ‘Trainspotting generation’ after the famous book and film by Irvine Welsh. But as pointed out by Ian Hamilton early on, this ageing cohort theory does problematic political work – becoming a convenient way for governments and governing bodies to absolve themselves of responsibility. It reduces a complex matter to that of a natural, even inevitable, process of ageing. I have heard many treatment providers talk about the increase in deaths in this way and it can preclude them from asking what more can be done.
This study was driven by a desire to speak to and focus in on the people behind these headlines and datasets and ask what more might be going on. While our recording systems can tell us what is going on – people who use heroin are ageing and deaths are increasing – they are less good at telling us why. In addressing the why, I spoke to those people deemed to be most at risk, older people who use heroin and other opioids.
Rather than viewing their age as a risk factor for overdose, participants pointed to a number of ways they saw their age (and experience) as protective, including:
1) having work and domestic responsibilities which meant they had to be careful over how much and frequently they used (illicit drugs);
2) their primary route of administration changing from injecting to smoking (associated with a reduced risk of overdose) due to the difficulty in finding a vein, but, also, with this;
3) the effects they desired shifting from the “hit” of the “old days” (“getting it in as quick as possible”) to a slower pleasure: “I’ve lost all my veins, and I kind of enjoy smoking anyway, I kind of like it, it's a bit more relaxed”;
4) having more acceptance towards their drug use and ‘user’ status meaning they were less likely to go “around and around on this wheel” of abstinence-work-relapse (as one participant put it), with the known risk of overdose following a period of abstinence, and lastly
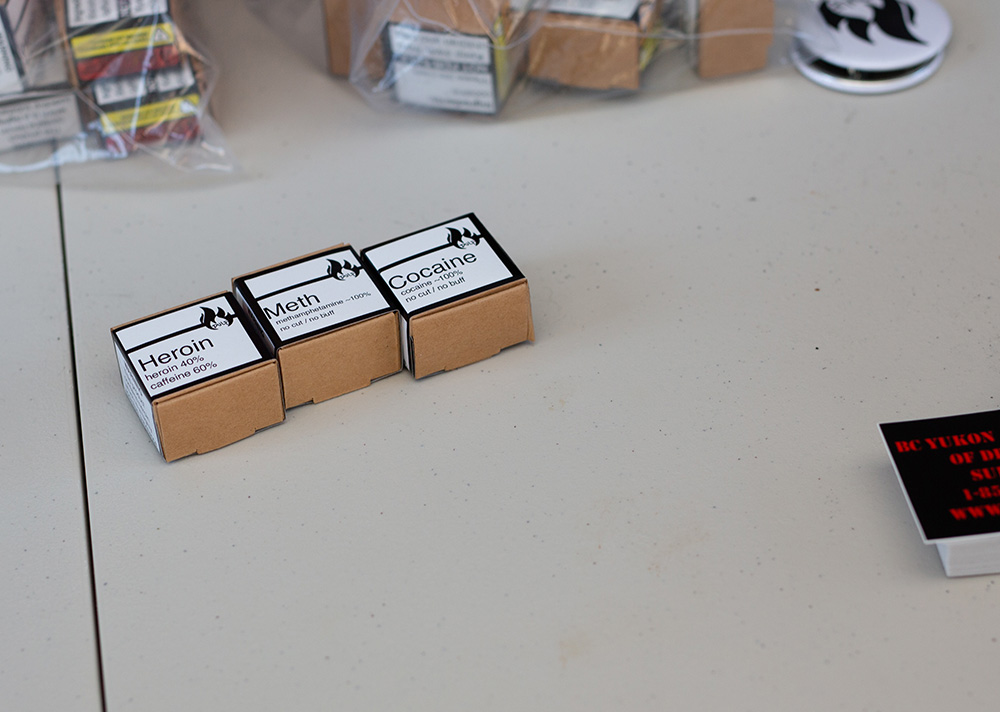
5) valuing and caring for their health, including having regular dealers who they knew and trusted.
Having looked at these factors that question older age as a given risk factor for overdose, the study turns to where participants, instead, see this risk of a drug-related death coming from.
"You know, you can listen to Public Health England and they say it’s because we’re all getting older and we all, kind of, have all of these other issues, like COPD [chronic obstructive pulmonary disease] and everything else, which is partly true, of course. But, I think there is another reason as well, and I think it’s the conversation that we’ve just had, with, you can’t really be open."
Here, this participant beautifully sums up what he and others told me was a wider problem with a punitive and inflexible treatment system where “you can’t be open” about your drug use. As a buprenorphine patient and daily illicit heroin user, this participant felt unable to discuss his ‘on top’ use with his drug worker (fearing an adjustment to his dose or collection regime – a fear that was realised for another participant in the study). This is a a catch-22 situation that many people who use drugs find themselves in! That is, they are in treatment for an issue they cannot talk about. How are treatment systems ever supposed to improve if service users are unable to talk about their illicit drug use (and, with this, how their current treatment may not be working)?
Moreover, even where some participants had spoken to doctors and drug workers about their illicit drug use and asked for a new approach (indeed, for some, at length and repeatedly – ‘‘Just saying, we require you to be drug free, but I’ve tried, it's not [working]. Can we try something else before I snuff it!?”), they felt ill-understood, ignored and even infantilised. Participants were frequently frustrated by the limited opiate-substitution treatment (OST) options on offer – methadone or buprenorphine – that they had tried at various times, and in varying ways over the last fifteen to twenty years. With this frustration came a despondency and fatalism that I say in the article could prove fatal as we know that overdose risk is heightened when people stop engaging with treatment. One participant described feeling resentful towards this treatment system that was not listening to her:
"I’m resentful because I’m fifty-six, I know what works for me. I know that heroin [diamorphine] or morphine is not in itself harmful, what is harmful is using stupid street drugs so please […] I’m not going to die of morphine, just work with me, give me what I need."
While, of course, this research does not attempt to represent all the views of older people who use heroin – taking place with a small number of people, at a particular time and location – it can start to complicate how we understand these rising death rates and ask questions over where we put our emphasis in terms of studying and responding to this crisis. Rather than seeing this as a natural process of ageing, which makes these deaths seem somewhat inevitable, the spotlight is turned onto our treatment and political systems that are failing to listen and respond to older peoples’ needs.
Therefore, in terms of what we can learn from this research, the message is clear: we need to listen more to older people who use opioids, realise their needs may be different to younger people who use drugs and honour these differences in our responses. This includes creating spaces where people can be listened to without fear of their treatment being affected. For people who have ‘tried everything’, there needs to be an expansion of opioid-substitution treatment, including morphine and diamorphine, and acceptance that abstinence may not be appropriate for everyone. Many older people have lived lives with opioids for a long time and giving them up may not feel possible or even desirable. Instead, treatment should be driven by the aspirations of the individuals involved, facilitating what they want out of life.
Fay Dennis is a researcher at Goldsmiths, University of London. More information about her work can be found here. Participant quotes are reproduced here from the original article, with permission from Wiley.